Overview
Ocular rosacea is a chronic inflammatory eye condition that occurs in people who have rosacea, a skin disorder that typically affects the face. In ocular rosacea, the inflammation extends to the eyes and eyelids, causing symptoms like dryness, redness, irritation, and gritty sensations.
It can occur before, during, or after facial rosacea appears, and in some cases, it may be the only visible manifestation of the disease. If left untreated, ocular rosacea can lead to serious complications, including corneal damage and vision loss.
What is Ocular Rosacea?
Ocular rosacea is the eye-related form of rosacea, a chronic inflammatory disorder that affects the sebaceous (oil) glands of the skin and eyes. In the eyes, the inflammation typically targets the eyelids, conjunctiva, meibomian glands, and occasionally the cornea.
The exact cause is unknown, but it’s believed to be related to a combination of genetic, environmental, and immune system factors. The condition is not contagious, but it tends to worsen over time without appropriate treatment.
Symptoms
Symptoms of ocular rosacea may vary in severity and can affect one or both eyes. Common symptoms include:
- Dry eyes or a burning sensation
- Redness in the eyes and eyelids
- Itching or irritation
- Gritty or foreign body sensation
- Blurred vision (especially in severe cases)
- Watery or teary eyes
- Light sensitivity (photophobia)
- Recurrent styes or eyelid swelling
- Red, thickened, or crusty eyelid margins
Symptoms can flare up periodically and may be worsened by sunlight, wind, alcohol, spicy food, or emotional stress.
Causes
The precise cause of ocular rosacea is not fully understood, but several contributing factors include:
- Chronic inflammation of the meibomian glands (oil glands in the eyelids)
- Overgrowth of skin bacteria or Demodex mites
- Abnormal immune response
- Genetic predisposition
- Environmental triggers, such as heat, cold, wind, or sun exposure
- Dysfunction of the sebaceous glands, leading to poor tear film quality
Many patients with ocular rosacea also have facial rosacea, but not all.
Risk Factors
You may be at increased risk of developing ocular rosacea if you:
- Have rosacea on the skin (especially affecting the cheeks and nose)
- Are aged between 30 and 60 years
- Have light skin, blue eyes, and blonde hair
- Have a family history of rosacea
- Are female (more likely to get rosacea) — though males may have more severe symptoms
- Live in extreme climates (hot, cold, or windy)
- Regularly consume spicy foods, alcohol, or hot beverages
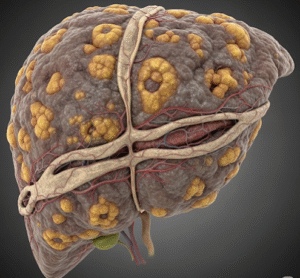
Complications
If untreated, ocular rosacea can lead to complications such as:
- Chronic dry eye disease
- Blepharitis (inflammation of the eyelids)
- Corneal inflammation (keratitis)
- Corneal ulcers or thinning, potentially resulting in vision loss
- Recurrent eye infections
- Iritis or scleritis in severe cases
Proper diagnosis and ongoing treatment are essential to prevent permanent damage.
Prevention
While ocular rosacea cannot be completely prevented, flare-ups can be minimized with lifestyle and hygiene measures:
- Use warm compresses to maintain eyelid hygiene
- Avoid known triggers (sunlight, spicy food, alcohol, etc.)
- Wear sunglasses to protect against UV and wind
- Use preservative-free artificial tears to manage dryness
- Avoid irritating eye makeup or facial products
- Practice good skin and eye hygiene
- Manage underlying facial rosacea with dermatologist guidance
Early and consistent treatment significantly improves long-term outcomes.
Treatment Options in Korea
South Korea offers excellent care for ocular rosacea through specialized ophthalmology and dermatology clinics that focus on chronic inflammatory eye diseases.
1. Diagnosis
- Comprehensive eye examination by an ophthalmologist
- Slit-lamp examination to evaluate eyelids, tear film, and cornea
- Assessment of meibomian gland function
- Diagnosis of concurrent facial rosacea
- Demodex mite testing (in some cases)
2. Medical Treatment
- Artificial tears: Preservative-free lubricating drops for dryness
- Eyelid hygiene: Warm compresses, lid scrubs, and eyelid wipes
- Topical antibiotics: Metronidazole or erythromycin gel for eyelid margins
- Oral antibiotics: Doxycycline or azithromycin to reduce inflammation
- Topical steroids (short-term use): To control severe inflammation
- Cyclosporine eye drops: For chronic inflammation
- Omega-3 fatty acid supplements: Improve meibomian gland function
3. In-office Procedures
- Meibomian gland expression
- Intense Pulsed Light (IPL) therapy for rosacea-related meibomian gland dysfunction
- LipiFlow thermal pulsation: Clears blocked oil glands
4. Integrated Care
In many Korean hospitals, patients can receive co-managed care from both dermatologists and ophthalmologists, ensuring holistic treatment of skin and eye symptoms.
5. Top Hospitals and Clinics in Korea
- Severance Eye Hospital – Ocular Surface Disease Center
- Samsung Medical Center – Eye and Skin Collaboration Clinic
- Asan Medical Center – Department of Ophthalmology and Dermatology
- Seoul National University Hospital – Dry Eye & Blepharitis Unit
- Kim’s Eye Hospital – Ocular Inflammation Clinic
These institutions offer:
- Advanced diagnostics and imaging tools
- Multidisciplinary treatment plans
- Modern therapies such as IPL and LipiFlow
- Multilingual support for international patients