Overview
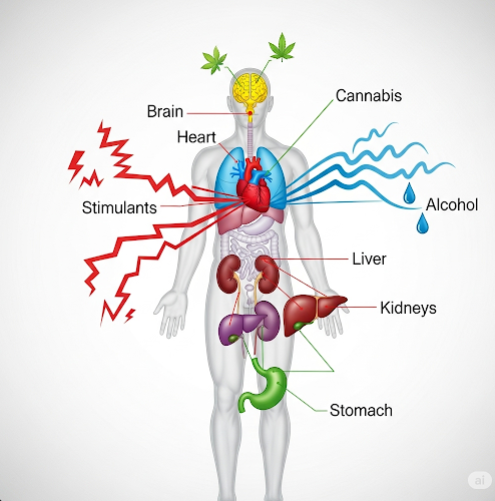
Polysubstance abuse refers to the simultaneous or sequential misuse of two or more psychoactive substances, such as alcohol, prescription drugs, illegal drugs, or other chemicals. Unlike single-substance addiction, polysubstance abuse involves multiple drugs being used to enhance effects, cope with withdrawal, or intensify intoxication. This behavior significantly increases the risk of overdose, physical and psychological damage, and treatment complexity.
It is especially common among young adults, individuals with co-occurring mental health disorders, and those in environments with easy access to multiple substances.
What is Polysubstance Abuse?
Polysubstance abuse occurs when an individual habitually uses more than one substance, often without a specific drug of choice. The substances may be used:
- Together (concurrently) to heighten or balance effects
- Alternately (sequentially) to avoid withdrawal or extend intoxication
Common combinations include:
- Alcohol + benzodiazepines
- Cocaine + heroin (“speedball”)
- Opioids + alcohol
- Stimulants + sedatives
- Prescription painkillers + marijuana or antidepressants
Polysubstance abuse often progresses to physical dependence, psychological addiction, and impaired daily functioning.
Symptoms
Symptoms of polysubstance abuse vary based on the substances used, but general signs may include:
- Frequent intoxication or hangovers
- Mood swings, aggression, or depression
- Slurred speech, impaired coordination, or confusion
- Risk-taking behaviors (e.g., unsafe sex, driving under the influence)
- Memory problems or blackouts
- Financial and legal issues
- Neglect of responsibilities at work, school, or home
- Social isolation or changes in peer groups
- Physical signs: weight changes, dilated pupils, tremors, track marks, poor hygiene
Withdrawal symptoms can be complex and severe due to overlapping effects of multiple substances.
Causes
Polysubstance abuse may be driven by a mix of psychological, environmental, and biological factors:
- Mental health disorders (e.g., depression, anxiety, PTSD)
- Peer pressure or social influence
- Chronic pain or undiagnosed physical illness
- Trauma or early-life abuse
- Genetic predisposition to addiction
- Availability of multiple drugs
- Desire to self-medicate or intensify effects
Often, individuals begin using one drug and add others to either counteract side effects or enhance euphoria.
Risk Factors
Several factors increase the risk of developing polysubstance abuse:
- History of mental illness or trauma
- Family history of substance use disorders
- Early exposure to drugs or alcohol
- Unstable social environment
- Lack of access to mental health support
- Adolescence or young adulthood
- Involvement in nightlife, club, or party culture
Healthcare providers must assess all potential substance interactions and underlying psychiatric issues.
Complications
Polysubstance abuse can lead to serious and life-threatening complications, including:
- Overdose, particularly from drug combinations (e.g., opioids and benzodiazepines)
- Respiratory depression, cardiac arrest, or coma
- Liver, kidney, or heart damage
- Severe withdrawal syndromes
- Cognitive impairment or memory loss
- Psychosis, anxiety, or mood disorders
- Infectious diseases (HIV, hepatitis C) from injection drug use
- Relationship breakdowns, unemployment, and homelessness
- High suicide risk
Treatment must address both the substance use and any co-occurring psychiatric or medical issues.
Prevention
Preventing polysubstance abuse involves a combination of education, early intervention, and community support:
- School and community education on drug interactions and risks
- Mental health screening and access to care
- Supportive family and social environments
- Monitoring and control of prescription medications
- Avoidance of high-risk settings where drug use is prevalent
- Encouraging open communication about stress and emotional challenges
- Promoting healthy coping strategies and self-esteem building in youth
Treatment Options in Korea
South Korea offers a growing number of integrated services for addiction recovery and mental health, with specialized programs in both public and private sectors.
1. Medical Detoxification
- Supervised withdrawal from multiple substances to manage withdrawal symptoms safely
- Hospital-based care for severe cases, especially involving alcohol, opioids, or benzodiazepines
- Use of medications like methadone, buprenorphine, or benzodiazepine tapers (depending on substances involved)
2. Inpatient and Outpatient Rehabilitation
- Inpatient rehab centers provide structured, intensive care
- Outpatient programs offer flexibility for those with work or family commitments
- Therapies used: Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Motivational Interviewing (MI)
3. Dual Diagnosis Treatment
- Addresses both mental health disorders and substance abuse
- Involves psychiatrists, psychologists, and addiction specialists
4. Support Groups and Counseling
- Group therapy, 12-step programs, or local support networks
- Family therapy to rebuild relationships and educate loved ones
- Aftercare planning for relapse prevention and social reintegration
5. Top Hospitals and Clinics in Korea
- National Center for Mental Health (Seoul)
- Samsung Medical Center’s Addiction Clinic
- Severance Hospital (Yonsei University)
- CHA Medical Center and other private psychiatry centers
These institutions offer:
- English-speaking staff for international patients
- Confidential and culturally sensitive care
- Customized recovery programs and long-term follow-up