Overview
Polioencephalitis is a rare and serious neurological condition that involves inflammation of the gray matter of the brain caused by the poliovirus. It is a severe manifestation of poliomyelitis, where the central nervous system (CNS), especially the brain, becomes inflamed. While the poliovirus primarily affects the spinal cord (as in paralytic polio), in polioencephalitis, the virus invades and damages brain tissue, potentially leading to brain dysfunction, neurological deficits, or death.
This condition is now extremely rare due to global polio vaccination efforts, but it remains a concern in unvaccinated or immunocompromised populations and areas where polio is still endemic.
What is Polioencephalitis?
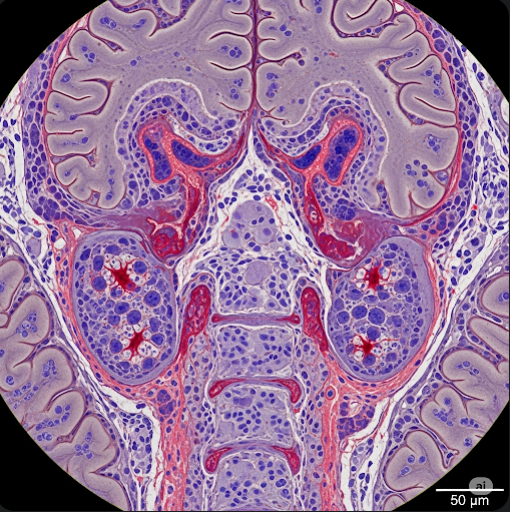
Polioencephalitis is a viral encephalitis caused by the poliovirus, a member of the Enterovirus genus. Unlike the more common spinal form of polio (which causes limb paralysis), polioencephalitis predominantly affects the brain’s gray matter, especially the brainstem, motor cortex, and other central areas.
It is considered a complication of poliomyelitis, particularly in its bulbar form, where the virus attacks brain centers that control essential functions like breathing and swallowing.
Symptoms
The symptoms of polioencephalitis often appear suddenly and severely, especially after initial flu-like symptoms of poliovirus infection. They may include:
- High fever
- Severe headache
- Stiff neck and back
- Nausea and vomiting
- Altered mental status (confusion, irritability, or delirium)
- Seizures
- Paralysis (especially of the respiratory muscles or cranial nerves)
- Difficulty swallowing or speaking
- Coma in advanced cases
- Respiratory failure due to brainstem involvement
These symptoms typically develop days after the onset of initial poliovirus infection and require immediate medical intervention.
Causes
The primary cause of polioencephalitis is infection with poliovirus, which enters the body via the oral-fecal route (usually through contaminated food or water). After initial replication in the throat and intestines, the virus can enter the bloodstream and, in rare cases, cross the blood-brain barrier to infect the central nervous system.
Key causes include:
- Wild poliovirus (WPV) – types 1, 2, and 3
- Oral polio vaccine (OPV) – very rarely, live attenuated strains may revert and cause neuroinvasion in immunocompromised individuals (vaccine-associated paralytic polio or VAPP)
Risk Factors
While polio is largely eradicated in many countries, the risk of polioencephalitis increases in the following groups:
- Unvaccinated individuals, especially in regions where polio is still endemic
- Immunocompromised individuals, such as those with HIV/AIDS or undergoing chemotherapy
- Infants and young children with incomplete polio immunization
- Travelers to polio-affected countries
- People in poor sanitation conditions
- Rare genetic immunodeficiencies that prevent viral clearance
Complications
Polioencephalitis can result in life-threatening and long-term neurological complications, including:
- Respiratory failure, requiring mechanical ventilation
- Cranial nerve palsies
- Permanent paralysis
- Swallowing and speech difficulties
- Brain damage
- Cognitive impairment or developmental delays
- Death, especially in untreated or severe cases
Early recognition and supportive treatment are critical to reduce mortality and improve outcomes.
Prevention
The most effective way to prevent polioencephalitis is complete vaccination against poliovirus. Prevention strategies include:
- Polio vaccination (IPV or OPV) according to national immunization schedules
- Booster doses for travelers to high-risk regions
- Improved sanitation and hygiene to prevent fecal-oral transmission
- Surveillance and rapid outbreak response in endemic areas
- Avoiding exposure to contaminated water or food in high-risk regions
In Korea, polio vaccination is part of the routine childhood immunization schedule, with a high national coverage rate.
Treatment Options in Korea
There is no specific antiviral treatment for polioencephalitis; care is focused on supportive and intensive care. South Korea provides world-class medical care for infectious and neurological conditions, including ICU-level support and rehabilitation.
1. Acute Care
- Hospitalization in intensive care for close monitoring
- Mechanical ventilation for respiratory muscle paralysis or brainstem involvement
- IV fluids, electrolyte balance, and nutritional support
- Antipyretics for fever and pain
- Seizure management with anticonvulsants
- Monitoring for complications such as pneumonia or autonomic instability
2. Rehabilitation
- Physical therapy to regain muscle strength and prevent contractures
- Speech therapy for bulbar symptoms
- Neurological rehabilitation for motor and cognitive recovery
- Psychological support for long-term disability adaptation
3. Long-Term Monitoring
- Neurologist follow-up for post-polio syndrome and residual weakness
- Respiratory therapy for chronic breathing issues
- Nutritional and swallowing support in severe cases
4. Korean Hospitals Offering Treatment
Top institutions like Asan Medical Center, Samsung Medical Center, Seoul National University Hospital, and Severance Hospital offer:
- Expert care in infectious neurology and intensive medicine
- Advanced imaging (MRI, CT) for CNS assessment
- Multidisciplinary teams including neurologists, infectious disease specialists, and rehabilitation therapists
- International patient services with English-speaking medical staff