Overview
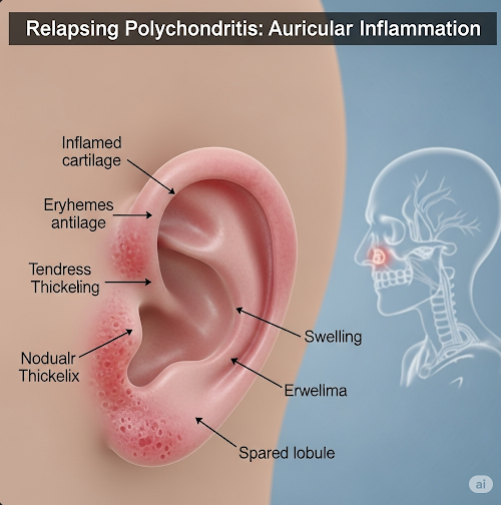
Polychondritis, more specifically Relapsing Polychondritis (RP), is a rare, chronic autoimmune disorder that primarily causes recurrent inflammation of cartilage throughout the body. It most commonly affects the ears, nose, joints, eyes, and respiratory tract, but may also involve other organs. Over time, inflammation can lead to progressive cartilage damage, deformities, and organ dysfunction. Although it is a lifelong condition, proper management can help reduce flare-ups and protect organ function.
What is Polychondritis?
Polychondritis is characterized by episodic and progressive inflammation of cartilaginous tissues. It is thought to be an autoimmune disease, where the body’s immune system mistakenly attacks its own cartilage and connective tissues.
Key types of cartilage affected include:
- Auricular cartilage (ears)
- Nasal cartilage (nose bridge)
- Laryngeal and tracheal cartilage (airways)
- Costal cartilage (rib cage)
- Articular cartilage (joints)
In severe cases, life-threatening airway obstruction or cardiovascular involvement may occur.
Symptoms
Symptoms of polychondritis vary depending on the organs involved and often come in flare-ups or relapses. Common symptoms include:
- Painful, red, swollen ears (sparing the earlobe) – hallmark sign
- Nasal inflammation – may cause a saddle-nose deformity over time
- Joint pain or arthritis
- Eye inflammation – conjunctivitis, scleritis, or uveitis
- Shortness of breath, cough, or hoarseness – due to airway inflammation
- Fatigue and fever
- Hearing loss, dizziness, or tinnitus
- Chest pain from costochondritis
Symptoms may worsen suddenly and then resolve, only to recur again later.
Causes
The exact cause of polychondritis is unknown, but it is believed to involve autoimmune mechanisms, where the body attacks proteins in cartilage.
Possible contributing factors:
- Autoimmune predisposition – may occur with other autoimmune diseases (e.g., lupus, rheumatoid arthritis, vasculitis)
- Genetic factors – though not clearly defined
- Environmental or infectious triggers – may play a role in initiating immune response
It is not contagious, and most cases are sporadic, with no known family history.
Risk Factors
Although polychondritis is rare, the following factors may increase risk:
- Age: Most commonly appears between ages 40 and 60
- Gender: Affects men and women equally
- Other autoimmune conditions: Present in up to one-third of cases
- History of connective tissue diseases (e.g., Sjögren’s syndrome, vasculitis)
Complications
If left untreated, relapsing polychondritis can lead to serious complications, especially if the airways, heart, or eyes are involved:
- Airway collapse or stenosis – life-threatening
- Hearing or vision loss
- Saddle-nose deformity – due to cartilage destruction
- Joint deformities
- Cardiac complications – such as aortic aneurysm, valve disease
- Kidney damage (rare)
- Permanent disfigurement of affected areas
- Increased infection risk due to immunosuppressive treatment
Prevention
There is no known way to prevent polychondritis since its exact cause is unknown. However, flare-ups can be minimized with early diagnosis and proper management:
- Avoid triggers of inflammation (e.g., infections, overexertion)
- Adhere to medication schedules
- Monitor symptoms and organ function regularly
- Routine check-ups with a rheumatologist or immunologist
- Report new symptoms early to prevent complications
Treatment Options in Korea
South Korea provides excellent care for autoimmune diseases like polychondritis, with access to rheumatology specialists, multidisciplinary teams, and advanced diagnostics.
1. Medication
- Corticosteroids (e.g., prednisone): First-line treatment for acute flare-ups
- Immunosuppressants:
- Methotrexate
- Azathioprine
- Cyclophosphamide (for severe disease)
- Biologic agents (e.g., TNF inhibitors, rituximab): In refractory or relapsing cases
- NSAIDs: For joint and musculoskeletal pain
- Topical or systemic treatments for eye involvement
2. Supportive Treatments
- Hearing aids or devices for ear damage
- Tracheostomy or airway stenting in cases of airway involvement
- Ophthalmologic treatment for eye inflammation
- Reconstructive surgery for nasal or ear deformities (in advanced cases)
3. Monitoring and Rehabilitation
- Regular lab tests to monitor inflammation markers and organ function
- Pulmonary function tests for airway involvement
- Cardiac imaging if heart complications are suspected
- Physical therapy for joint involvement and mobility preservation
4. Best Hospitals in Korea
Hospitals such as Asan Medical Center, Samsung Medical Center, Seoul National University Hospital, and Severance Hospital offer:
- Experienced rheumatology and immunology teams
- Multispecialty clinics for ENT, ophthalmology, and cardiology support
- Advanced imaging and diagnostics
- English-speaking international care services