Overview
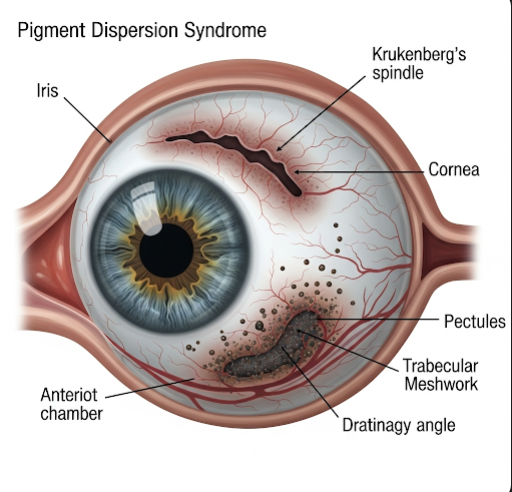
Pigment Dispersion Syndrome (PDS) is an eye condition in which pigment granules, normally found on the back of the iris, are released into the clear fluid inside the eye (aqueous humor). These granules can accumulate in various parts of the eye, particularly the drainage canals, and may lead to elevated intraocular pressure (IOP), increasing the risk of a serious condition called pigmentary glaucoma. Early diagnosis and monitoring are crucial to prevent long-term damage to vision.
What is Pigment Dispersion Syndrome?
Pigment Dispersion Syndrome is a disorder that affects the iris and intraocular structures, leading to the shedding of melanin pigment from the iris. These tiny pigment particles float in the aqueous humor and can settle in various parts of the eye, including the trabecular meshwork — the eye’s natural drainage system. If this drainage becomes clogged, pressure inside the eye can rise, which may damage the optic nerve and result in pigmentary glaucoma.
PDS typically develops in young to middle-aged adults and is more common in people with myopia (nearsightedness).
Symptoms
Many individuals with Pigment Dispersion Syndrome do not experience symptoms and may only be diagnosed during a routine eye exam. However, when symptoms do occur, they may include:
- Blurry vision
- Halos around lights
- Eye discomfort after exercise or pupil dilation
- Mild eye pain or pressure
- Intermittent vision disturbances
- Seeing floaters
- Elevated intraocular pressure (detected by an eye specialist)
Causes
The exact cause of Pigment Dispersion Syndrome is not fully understood, but several mechanisms have been identified:
- Anatomical predisposition: In PDS, the iris bows backward, causing it to rub against the lens zonules (fibers supporting the lens), releasing pigment
- Genetics: There may be a hereditary component, though specific genes are still under study
- Physical activity: Vigorous exercise or activities that dilate the pupil can increase the release of pigment
- Eye structure: Common in individuals with deep anterior chambers and large pupils
- Age-related changes: PDS often stabilizes or becomes less active as individuals age
Risk Factors
Several factors can increase the risk of developing Pigment Dispersion Syndrome:
- Age: Most common between 20–40 years old
- Sex: Slightly more prevalent in males
- Refractive error: Higher in individuals with moderate to high myopia
- Race: More commonly diagnosed in people of European descent
- Family history of PDS or pigmentary glaucoma
- Athletic activity: Intense sports or physical activity may trigger pigment release
Complications
The primary complication of PDS is the development of pigmentary glaucoma, a form of secondary open-angle glaucoma that can lead to irreversible vision loss. Other potential complications include:
- Elevated intraocular pressure
- Optic nerve damage
- Visual field loss
- Decreased peripheral vision
- Progression to chronic glaucoma if untreated
- Cataract formation (in rare advanced cases)
Regular eye exams are essential to detect these issues early and manage them appropriately.
Prevention
While Pigment Dispersion Syndrome itself cannot be completely prevented, the risk of complications can be reduced by:
- Regular comprehensive eye exams, especially for high-risk individuals
- Avoiding excessive physical strain or exercises that involve jarring head movements
- Wearing protective eyewear during sports to avoid trauma
- Managing myopia and discussing risks with your eye care provider
- Monitoring IOP levels regularly once diagnosed
- Early intervention to control pigment release or drainage blockage
Treatment Options in Korea
South Korea is a leading destination for advanced ophthalmologic care, including the diagnosis and treatment of Pigment Dispersion Syndrome and pigmentary glaucoma. Treatment options include:
- Observation and monitoring: In early or mild cases without elevated IOP, regular monitoring may be all that’s needed
- Medicated eye drops: To reduce intraocular pressure or limit pigment dispersion
- Beta-blockers (e.g., timolol)
- Prostaglandin analogs (e.g., latanoprost)
- Carbonic anhydrase inhibitors
- Laser therapy:
- Laser Peripheral Iridotomy (LPI): May help flatten the iris and reduce pigment shedding
- Selective Laser Trabeculoplasty (SLT): Improves drainage and reduces IOP
- Surgical treatment: In advanced or treatment-resistant cases, filtering surgery such as trabeculectomy may be recommended
- Advanced diagnostics: Optical Coherence Tomography (OCT), visual field testing, and gonioscopy are available at all major eye centers
- Specialized glaucoma clinics: Hospitals like Samsung Medical Center, Seoul National University Hospital, and Kim’s Eye Hospital offer personalized glaucoma management, with English-speaking staff and medical tourism services for international patients
Korea’s ophthalmology sector combines precision diagnostics, minimally invasive laser treatments, and expert surgical care to manage conditions like Pigment Dispersion Syndrome effectively and safely.