Virtual reality (VR) is gradually being adopted in Korea as a tool to enhance rehabilitation and recovery across neurological, musculoskeletal, and cognitive domains. Korean experts see it as a way to increase engagement, provide more intensive training, and deliver therapy beyond the walls of the clinic. Below is a look at how VR is being used in Korea’s recovery programs, what evidence exists, challenges, and future directions.
🧩 Current Applications & Clinical Use in Korea
Stroke Rehabilitation – Upper Limb Motor Recovery
One of the better documented areas in Korean research is VR for upper limb motor rehabilitation after stroke. VR systems allow patients to perform repeated, interactive tasks tailored in difficulty, with real-time feedback, which supports neural plasticity and motor relearning.
Because standard physical therapy often becomes monotonous, VR adds gamification and engagement, encouraging more repetitions of movement—key for recovery.
Therapist Adoption & Attitudes Survey
A national survey of physical therapists (PTs) and occupational therapists (OTs) in Korea assessed attitudes toward VR/active video game–based rehabilitation. Therapists with prior VR experience showed more favorable perceptions and greater intent to adopt VR in practice. The biggest barriers cited were lack of funding and technical support for VR setup.
This suggests that while professionals see the potential, practical and resource constraints slow adoption.
Musculoskeletal & Orthopedic Rehabilitation
Though not always specific to Korea, recent reviews in orthopedic settings show VR is being used to rehabilitate joint function, strength, balance, and mobility after orthopedic injuries or surgeries. These findings are transferable to Korean clinics, which are exploring VR for post-surgical rehab of knees, spine, and limbs.
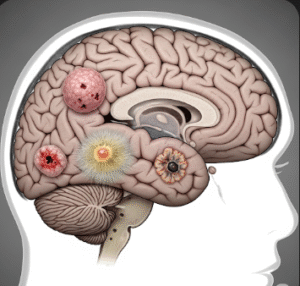
Neurosurgical / Neurotrauma Recovery
Some exploratory VR programs are being applied early in neurosurgical or neurotrauma inpatient settings. For example, in other countries, VR is used daily postoperatively to engage patients in simple motor or cognitive tasks as soon as safety allows. While not uniquely Korean, this approach is part of the frontier that Korean centers are likely watching or piloting.
🎯 Benefits & Strengths of VR in Recovery Programs
- Higher engagement & motivation: Patients often respond better to immersive, game-like tasks than repetitive drills—improving adherence.
- Adaptive difficulty & feedback: VR allows real-time adjustment of task difficulty and gives immediate visual or auditory feedback, which helps patients correct movement and progress.
- Safe, simulated environments: Activities of daily living, balance challenges, or obstacle negotiation can be replicated virtually in a controlled risk environment.
- Standardized and repeatable therapy: VR enables consistent delivery of tasks across sessions, reducing variability.
- Potential for home-based rehabilitation: Telerehabilitation combined with VR allows patients to continue therapy at home, extending recovery beyond clinic hours.
- Data tracking and analytics: Movement metrics, speed, accuracy, and progression can be quantified, giving therapists objective insight into patient progress and need for adjustment.
🚧 Challenges & Barriers in Korean Context
- Cost and Infrastructure: High-quality VR systems and associated sensors or motion capture systems are expensive, and many clinics or smaller institutions may lack funding to purchase or maintain them.
- Technical expertise & support: Clinics often lack staff who are comfortable with VR setup, calibration, troubleshooting, or integrating it with existing rehabilitation workflows.
- Therapist confidence & training: Some therapists express low self-efficacy using VR—especially those without prior experience. Survey data showed those without VR experience rated lower in domains related to adopting it.
- Patient factors: Some older or severely impaired patients may experience motion sickness, fatigue, or difficulty with VR headsets.
- Limited evidence in certain domains: While data is growing in stroke and motor rehab, there is less strong evidence for fine motor control, complex cognition, or varied patient populations.
- Interoperability / integration: Integrating VR systems with hospital information systems or clinical documentation can be challenging.
- Regulation & reimbursement: VR-based therapies may not yet be covered by insurance or national health systems, which limits adoption.
🔭 Future Prospects & Directions in Korea
- Hybrid VR + AI systems: Combining VR with artificial intelligence to customize therapy paths, predict progress, or suggest adaptive task sequences.
- Wearable + VR synergy: Use of wearable sensors (inertial measurement units, EMG) integrated with VR to improve accuracy of motion tracking and feedback.
- Home VR rehabilitation platforms: More systems designed for safe home use under clinician monitoring, especially for chronic conditions or rural areas.
- Gamification & social VR: Multiplayer rehabilitation games where patients can compete or collaborate, which may increase motivation.
- Expanding indications: Beyond stroke or orthopedic rehab, VR might be used for balance disorders, Parkinson’s disease, vestibular rehab, and cognitive rehabilitation after brain injury.
- National standardization & guidelines: Korea may develop standards or guidelines for VR rehabilitation use, quality assurance, and outcome tracking.
- Larger clinical trials: More randomized controlled trials in Korean populations to validate efficacy, cost-effectiveness, and optimal protocols.