Overview
Paracoccidioidomycosis is a rare but serious fungal infection caused by the Paracoccidioides species, primarily Paracoccidioides brasiliensis and Paracoccidioides lutzii. It mainly affects the lungs but can spread to other parts of the body, including the skin, mucous membranes, and lymph nodes. This infection is endemic in some parts of Latin America, especially Brazil, but may appear in other regions through travel or migration. It is a chronic condition and requires long-term treatment.
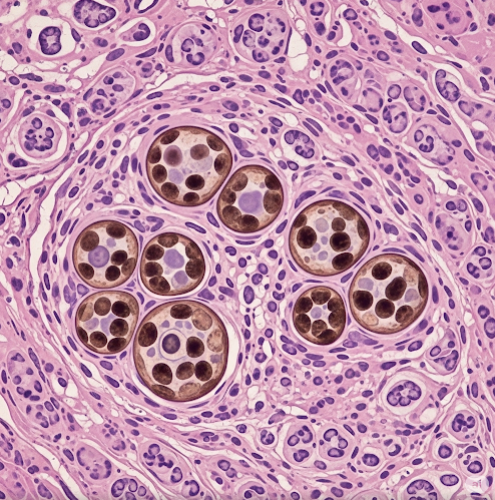
What is Paracoccidioidomycosis?
Paracoccidioidomycosis (PCM), also known as South American blastomycosis, is a systemic fungal disease that begins when a person inhales the fungal spores from the environment, usually from soil. After entering the body through the respiratory tract, the fungus can remain dormant for years before causing symptoms. In some individuals, especially those with weakened immune systems, the infection spreads to other organs and tissues.
There are two main clinical forms:
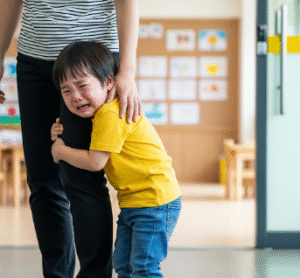
- Acute/Subacute Form: Affects children and young adults, involving multiple organs such as the lymph nodes, liver, and spleen.
- Chronic Form: Common in adult men, often involves the lungs, mouth, skin, and lymph nodes.
Symptoms
Symptoms vary based on the form of the disease, but common signs include:
- Chronic cough
- Shortness of breath
- Weight loss
- Fever and fatigue
- Skin ulcers or nodules
- Painful mouth or throat sores
- Swollen lymph nodes
- Difficulty swallowing (in mucosal involvement)
- Enlarged liver or spleen in acute forms
Symptoms often mimic tuberculosis or other respiratory diseases, making diagnosis challenging.
Causes
Paracoccidioidomycosis is caused by inhaling spores of Paracoccidioides fungi, which live in moist soil, particularly in rural or agricultural regions. The spores enter the lungs and can disseminate to other body parts through the bloodstream or lymphatic system.
The fungus is not contagious from person to person.
Risk Factors
People at higher risk include:
- Farmers or rural workers exposed to soil
- People living in endemic areas, especially Brazil, Colombia, and Venezuela
- Males aged 30 to 60 years (the chronic form is rare in women)
- Individuals with weakened immune systems (due to HIV/AIDS, cancer, or malnutrition)
- Those with a history of long-term exposure to soil without protective measures
Complications
If left untreated or if diagnosis is delayed, complications may include:
- Severe lung damage and respiratory failure
- Disfigurement due to skin or mucosal lesions
- Gastrointestinal or neurological involvement (in rare cases)
- Malnutrition and weight loss
- Opportunistic infections in immunocompromised individuals
- Death, in severe untreated cases
Prevention
Since there’s no vaccine, prevention relies on minimizing exposure and improving early diagnosis:
- Use of protective equipment (masks, gloves) when working with soil in endemic regions
- Avoiding known high-risk environments, especially during construction or deforestation
- Prompt diagnosis and treatment of respiratory symptoms in travelers returning from endemic areas
- Public health education in rural farming communities
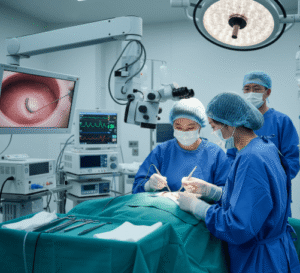
Treatment Option in Korea
While paracoccidioidomycosis is extremely rare in Korea, treatment is available in major infectious disease and pulmonary centers. Once diagnosed, Korean hospitals follow global standards for antifungal therapy.
1. Antifungal Medications
The most common treatments include:
- Itraconazole – oral antifungal used for mild to moderate cases
- Amphotericin B – used in severe or disseminated cases; usually administered intravenously in a hospital setting
- Sulfamethoxazole-trimethoprim – may also be used, especially for long-term therapy
Treatment duration is typically 6 months to 2 years, depending on the severity.
2. Supportive Care
Nutritional support, pulmonary rehabilitation, and wound care may be provided in advanced centers like Seoul National University Hospital or Asan Medical Center.
3. Monitoring and Follow-Up
Regular imaging (chest X-rays, CT scans), blood tests, and symptom tracking are essential. Korea’s healthcare system allows for efficient follow-up through both public and private clinics.
4. Travel-Related Expertise
In Korea, travel and tropical medicine clinics (e.g., in Severance Hospital or Samsung Medical Center) are equipped to diagnose and treat rare imported fungal infections like PCM.
Although not endemic to Korea, the country’s high-level infectious disease infrastructure ensures that rare infections are identified and managed with international best practices.