Overview
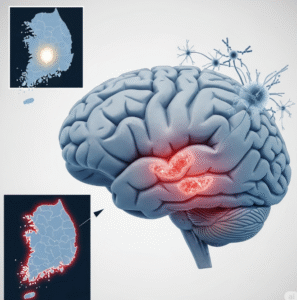
Systemic onset juvenile arthritis (SOJA), also known as systemic juvenile idiopathic arthritis (sJIA), is a rare but serious form of juvenile arthritis that affects children. Unlike other types, it begins with systemic (whole-body) symptoms such as fever, rash, and inflammation of internal organs, before joint pain becomes evident. In Korea, early detection and advanced immunologic treatments have improved the outcomes for children affected by this condition.
What is Systemic Onset Juvenile Arthritis?
Systemic onset juvenile arthritis is a subtype of juvenile idiopathic arthritis (JIA) that affects children under the age of 16. It is characterized by inflammation in one or more joints, accompanied or preceded by systemic symptoms like daily fever spikes and rash.
sJIA is considered an autoinflammatory disease, meaning it stems from an abnormal activation of the immune system, rather than being triggered by external factors such as infections. It can range from mild to severe and may lead to long-term joint damage if untreated.
Symptoms
- Daily high fevers (often in the late afternoon or evening)
- Evanescent salmon-pink rash (comes and goes with fever)
- Joint swelling and stiffness (often multiple joints)
- Fatigue and malaise
- Swollen lymph nodes
- Hepatosplenomegaly (enlarged liver/spleen)
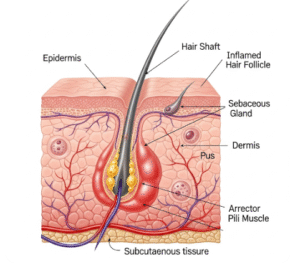
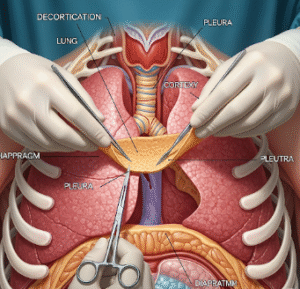
- Serositis (inflammation of membranes lining lungs or heart)
- Weight loss and poor appetite
In some children, joint symptoms may appear weeks or months after the systemic signs begin.
Causes
The exact cause of systemic juvenile arthritis is unknown, but it is believed to involve dysregulation of the innate immune system. Genetic factors and immune pathway abnormalities (especially involving interleukin-1 and interleukin-6) play a central role.
Unlike other autoimmune conditions, sJIA is not typically associated with autoantibodies, suggesting it is more autoinflammatory in nature.
Risk Factors
- Age: Typically occurs in children under 16 years of age
- Genetics: Certain genetic markers may increase susceptibility
- Sex: Affects both boys and girls equally (unlike other JIA subtypes)
- Environmental triggers: Though unclear, infections may sometimes precede onset
Complications
If not treated properly, sJIA can lead to:
- Chronic joint inflammation and damage
- Growth retardation in children
- Anemia and fatigue
- Macrophage activation syndrome (MAS): a potentially fatal hyperinflammatory complication
- Osteoporosis due to long-term corticosteroid use
- Decreased quality of life and psychosocial challenges
Prevention
There is currently no known way to prevent systemic onset juvenile arthritis. However, early diagnosis and treatment can greatly reduce complications and disease progression.
- Educate caregivers on early signs
- Encourage routine pediatric checkups
- Monitor children with unexplained fevers and rashes
Treatment Options in Korea
South Korea offers world-class care for pediatric autoimmune and autoinflammatory diseases, including systemic JIA. Tertiary care hospitals are equipped with pediatric rheumatology specialists and the latest treatment options.
Diagnosis
- Detailed clinical evaluation
- Blood tests:
- Elevated ESR, CRP, and ferritin
- Anemia and leukocytosis
- Negative rheumatoid factor (RF) and ANA
- Imaging:
- Ultrasound or MRI to detect joint inflammation
- Chest X-ray or echocardiogram (if serositis suspected)
- Exclusion of infections, leukemia, and other causes
Medications
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Often used initially to reduce fever and pain
- Corticosteroids
- Prednisone is commonly used to control severe inflammation
- Close monitoring due to potential side effects in children
- Disease-Modifying Antirheumatic Drugs (DMARDs)
- Methotrexate is often prescribed for joint symptoms
- Biologic Therapies
Korea is at the forefront of biologic treatment for pediatric patients, including:- IL-1 inhibitors (e.g., anakinra, canakinumab)
- IL-6 inhibitors (e.g., tocilizumab – widely available in Korea)
These are highly effective in controlling systemic symptoms and preventing joint damage.
- Treatment for MAS (Macrophage Activation Syndrome)
- Immunosuppressants like cyclosporine, high-dose steroids, or biologics
Supportive Care
- Physical therapy to maintain joint mobility
- Psychological counseling for children and families
- Nutritional support to combat growth issues
- Regular growth and development monitoring
Top Hospitals in Korea for Pediatric Rheumatology
- Seoul National University Children’s Hospital – Pediatric Rheumatology Center
- Asan Medical Center – Children’s Hospital – Comprehensive care for juvenile arthritis
- Samsung Medical Center – Department of Pediatric Immunology and Rheumatology
- Yonsei Severance Children’s Hospital
Access and Insurance
- Covered under National Health Insurance Service (NHIS)
- Rare Disease Registry in Korea provides additional subsidies for chronic pediatric conditions
- Hospitals offer long-term care plans and family education services