What it is
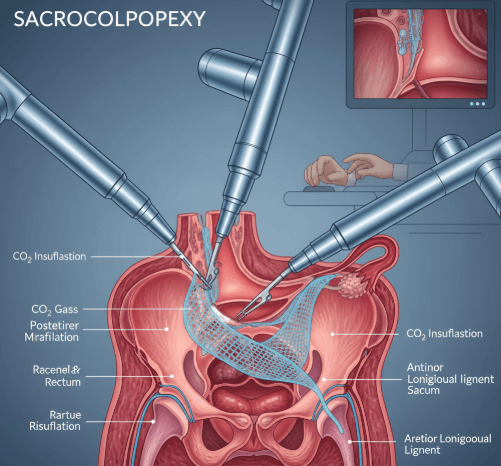
Sacrocolpopexy is a surgical procedure to correct vaginal vault prolapse, a condition where the top of the vagina sags or drops after hysterectomy. During the surgery, the vagina is lifted and attached to the sacrum (lower spine) using a synthetic mesh, restoring normal support and preventing the vault from collapsing into the vaginal canal.
In Korea, sacrocolpopexy is performed using laparoscopic or robotic-assisted techniques, which allow surgeons to carry out the repair with high precision, minimal scarring, and faster recovery compared to open surgery.
➡️ Key facts about sacrocolpopexy:
- Considered the gold standard surgery for vaginal vault prolapse
- Provides long-lasting results with low recurrence rates
- Can be combined with other prolapse or incontinence surgeries
Why it’s done
Vaginal vault prolapse can cause discomfort, urinary and bowel issues, and sexual dysfunction. Sacrocolpopexy is performed to restore anatomy and improve quality of life.
✔️ Medical reasons for sacrocolpopexy include:
- Vaginal bulge sensation or visible protrusion
- Pelvic pressure or heaviness
- Urinary incontinence or incomplete bladder emptying
- Bowel problems such as constipation or incomplete evacuation
- Painful intercourse or reduced sexual function
✔️ Benefits of sacrocolpopexy:
- Provides durable pelvic support
- Improves bladder and bowel function
- Relieves pelvic pressure and bulge symptoms
- Enhances sexual health and confidence
- Long-term success rates higher than many vaginal repairs
Alternatives
Not all women with vault prolapse need sacrocolpopexy. Alternatives may be considered depending on symptoms and severity.
🔹 Pelvic floor therapy:
- Kegel exercises, biofeedback, and electrical stimulation
- Strengthens muscles to support mild prolapse
🔹 Pessaries:
- Vaginal devices inserted to support the vagina
- Non-surgical option for women unable or unwilling to undergo surgery
🔹 Other surgical options:
- Sacrospinous ligament fixation (attaching vagina to pelvic ligaments)
- Uterosacral ligament suspension (using natural tissue for support)
- These may be less invasive but often have higher recurrence than sacrocolpopexy
🔹 Observation:
- Asymptomatic or mild prolapse may only need monitoring
Preparation
Preparation ensures safe surgery and better recovery.
➡️ Medical preparation:
- Pelvic exam and imaging (ultrasound or MRI) to evaluate prolapse severity
- Urodynamic testing if incontinence is suspected
- Blood tests and overall health screening before anesthesia
➡️ Personal preparation:
- Stopping blood thinners or certain medications if advised
- Fasting for 6–8 hours before general anesthesia
- Arranging for short hospital stay (usually 2–3 days)
➡️ Mental preparation:
- Understanding surgery involves synthetic mesh placement
- Emotional readiness for lifestyle modifications after surgery
- Counseling to address intimacy, body image, and long-term outcomes
How it’s done
Sacrocolpopexy in Korea is usually performed using minimally invasive methods for precision and comfort.
✔️ Step 1 – Anesthesia
- General anesthesia administered for pain-free surgery
✔️ Step 2 – Creating access
- Small incisions made in the abdomen for laparoscope or robotic instruments
- Carbon dioxide gas used to inflate abdomen for visibility
✔️ Step 3 – Vaginal vault support
- Synthetic mesh attached to the top of the vagina
- Mesh then anchored to the sacrum with sutures for long-term support
✔️ Step 4 – Completion
- Mesh covered with peritoneum (abdominal lining) to reduce complications
- Incisions closed with sutures or surgical glue
✔️ Duration:
- Surgery typically lasts 2–3 hours
- Hospital stay: 1–3 days for minimally invasive, longer for open surgery
Recovery
Recovery from sacrocolpopexy is generally smooth with Korea’s minimally invasive techniques.
➡️ Immediate recovery:
- Abdominal soreness, mild bloating, or vaginal pressure
- Bladder catheter may remain temporarily after surgery
- Hospital monitoring for infection, bleeding, or urinary issues
➡️ Physical recovery:
- Return to light activities in 2–3 weeks
- Full recovery in 6–8 weeks
- Avoiding heavy lifting, strenuous exercise, and sexual activity until cleared by the doctor
➡️ Emotional recovery:
- Relief from prolapse symptoms improves confidence and daily life
- Counseling may be beneficial for women adjusting to mesh implants or body image changes
- Sexual function often improves but requires gradual resumption
➡️ Key recommendations:
- Adequate hydration and a high-fiber diet to avoid constipation
- Performing pelvic floor therapy after healing to prevent recurrence
- Attending all follow-up visits for mesh placement monitoring
Treatment option in Korea
Korea is a global leader in urogynecology and minimally invasive pelvic surgery, making it a top choice for sacrocolpopexy.
✔️ Hospital facilities:
- Equipped with robotic-assisted surgical systems for precision sacrocolpopexy
- Specialized urogynecology centers offering advanced prolapse and incontinence treatments
- State-of-the-art recovery and monitoring systems
✔️ Medical expertise:
- Surgeons highly skilled in complex prolapse repair and mesh-based surgeries
- High success rates with low recurrence risk
- Personalized surgical planning based on patient’s age, health, and prolapse severity
✔️ Postoperative care:
- Structured follow-up care to monitor mesh placement and healing
- Integration of pelvic floor rehabilitation into recovery
- Counseling for lifestyle adjustments and sexual health
✔️ Cultural aspect:
- Korean healthcare emphasizes privacy, comfort, and holistic recovery
- Women often access Sanhujoriwon-style centers after surgery for guided nutrition, rest, and rehabilitation
➡️ Highlight: Sacrocolpopexy in Korea provides state-of-the-art surgical precision, advanced mesh repair, and holistic recovery programs, ensuring women regain pelvic stability, confidence, and long-term health.