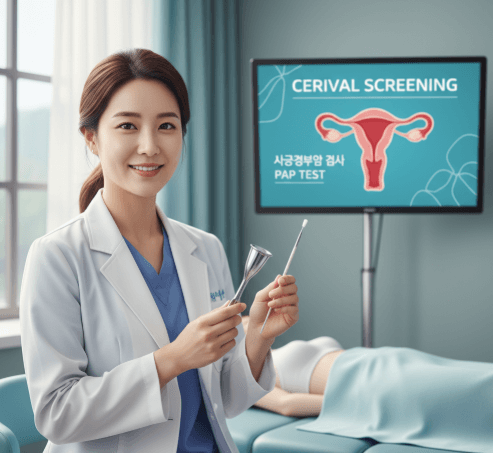
What it is
- ➤ A Pap smear (Pap test) is a preventive screening test that collects cells from the cervix (the opening of the uterus) to check for abnormal changes.
- ➟ The aim is to detect pre-cancer or cancer early, often before symptoms appear.
- ✦ Two main formats:
- ▪ Conventional Pap test → cells smeared on a slide.
- ▪ Liquid-based cytology (LBC) → cells placed in liquid for clearer, more accurate analysis (widely used in Korea).
- ➤ Often paired with HPV DNA testing for higher accuracy.
- Important: The Pap smear only screens for cervical abnormalities—not ovarian or uterine cancer.
Why it’s done
- ➤ Primary goal: Prevent cervical cancer by catching precancerous changes (CIN).
- ➟ Indications:
- ▪ Routine screening for individuals with a cervix.
- ▪ Follow-up after abnormal results or cervical treatment.
- ▪ Higher-risk groups (immunosuppressed, persistent HPV).
- ✦ Benefits:
- ✅ Detects early, highly treatable changes.
- ✅ Takes just 2–5 minutes, low discomfort, low risk.
- ⟶ Limitations:
- ▪ Not 100% perfect → false positives or negatives possible.
- ▪ Requires regular intervals for reliability.
- Bold takeaway: Regular screening drastically lowers cervical cancer deaths.
Alternatives
- ➤ HPV DNA testing: Detects high-risk HPV strains. More sensitive than Pap alone.
- ➟ Co-testing (Pap + HPV): Highly effective, may allow longer screening intervals if negative.
- ✦ VIA (Visual Inspection with Acetic Acid): Used in low-resource settings, not common in Korea.
- ⟶ Colposcopy: Not a screening option; it’s a follow-up diagnostic test.
- Important: Even if vaccinated for HPV, you still need Pap or HPV screening.
Preparation
- ➤ Schedule mid-cycle (day 10–20 of menstrual cycle).
- ✦ Avoid for 24–48 hours before test:
- ▪ Intercourse
- ▪ Vaginal creams or medicines (unless prescribed)
- ▪ Tampons
- ▪ Douching (never recommended)
- ➟ Tell your clinician if you:
- ▪ Might be pregnant
- ▪ Recently had infections or procedures
- ▪ Take medications affecting immunity or bleeding
- → Bring: ID, past test results, list of medications.
- Important: If you have heavy bleeding, reschedule for best accuracy.
How it’s done
- ➤ Check-in & consent: Quick medical history and confirmation.
- ➟ During procedure (2–5 minutes):
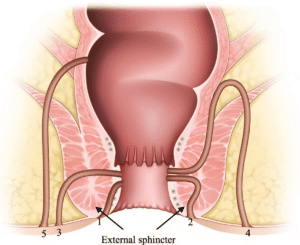
- ▪ A speculum gently opens the vagina.
- ▪ A small spatula/brush collects cervical cells.
- ▪ Sample placed on a slide or in liquid vial.
- ✦ Optional: HPV swab may also be collected.
- → What you feel: Pressure and a brushing sensation—brief but tolerable.
- After: Speculum removed, you return to normal activities immediately.
- Important: Clinics in Korea follow strict sterilization and identity checks.
Recovery
- ➤ Right after: Normal activities are safe.
- ✦ Possible minor effects:
- ▪ Mild spotting
- ▪ Slight cramps
- ➟ If spotting occurs: Avoid tampons, intercourse, or vaginal products for 24h.
- → Results:
- ▪ Normal → continue screening as advised.
- ▪ Abnormal (ASC-US, LSIL, HSIL, HPV+) → repeat test, HPV typing, or colposcopy.
- ⟶ Seek care urgently if:
- ➤ Heavy bleeding
- ➤ Severe pain
- ➤ Fever or foul discharge
- Important: Keep a personal record of results and never skip follow-ups.
Treatment option in Korea
- ➤ Where to go:
- ▪ University hospitals in Seoul, Busan, Incheon, Daegu, etc.
- ▪ Specialized women’s centers with international patient services.
- ✦ Why Korea:
- ▪ Advanced cytology labs with liquid-based cytology & HPV genotyping.
- ▪ Same-day packages (consultation + Pap + HPV + ultrasound).
- ▪ Transparent pricing and English-language support.
- ➟ If abnormal results:
- ▪ Colposcopy + biopsy for diagnosis.
- ▪ Cryotherapy or laser therapy for mild changes.
- ▪ LEEP or conization for high-grade lesions.
- ▪ Oncology care if cancer is confirmed.
- ⟶ For international patients:
- ▪ Send prior records ahead of time.
- ▪ Plan 1–3 days for screening & results.
- ▪ Request reports in English.
- Important: Korea’s system is efficient, but your consistency with follow-up is what ensures success.