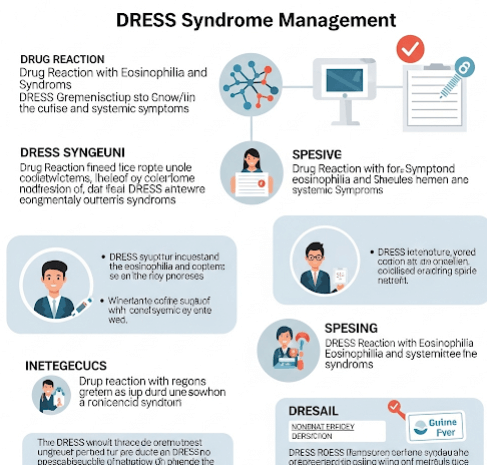
What it is
➝ DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) syndrome is a severe, potentially life-threatening drug hypersensitivity reaction.
➝ It typically occurs 2–8 weeks after starting the offending drug and presents with widespread skin eruption, fever, lymphadenopathy, eosinophilia, and involvement of internal organs (liver, kidneys, lungs, heart).
➝ Common culprit drugs include anticonvulsants (phenytoin, carbamazepine, lamotrigine), allopurinol, sulfonamides, antibiotics, and antituberculosis agents.
➝ Management requires early recognition, immediate withdrawal of the culprit drug, systemic therapy, and long-term monitoring for organ damage.
➝ In Korea, treatment is coordinated in dermatology, internal medicine, and allergy-immunology centers due to the multisystem involvement.
Why it’s done
→ To prevent progression to multi-organ failure, which can be fatal.
→ To relieve systemic symptoms such as high fever, severe rash, and lymphadenopathy.
→ To manage internal organ inflammation (especially hepatitis, nephritis, pneumonitis, myocarditis).
→ To reduce risk of relapse and autoimmune sequelae, which can occur months later.
→ In Korea, DRESS management is emphasized as a medical emergency requiring inpatient monitoring.
Alternatives / Treatment Approaches
→ Immediate drug withdrawal (dechallenge): The single most important first step.
→ Systemic corticosteroids:
- Prednisone 1 mg/kg/day (or equivalent), tapered slowly over weeks to months.
- Intravenous methylprednisolone pulses in severe cases.
→ Immunosuppressive or adjunctive therapies:
- Cyclosporine (used increasingly as a steroid-sparing option).
- Intravenous immunoglobulin (IVIG) in selected refractory cases.
- Mycophenolate or cyclophosphamide in rare severe cases.
→ Supportive care:
- Antihistamines and emollients for skin symptoms.
- IV fluids, nutritional support, and infection control.
- Organ-specific management (e.g., hepatology for liver involvement).
Preparation
→ Confirm diagnosis with clinical scoring systems (e.g., RegiSCAR criteria).
→ Baseline investigations include CBC with differential, liver and renal function tests, electrolytes, urinalysis, chest imaging, and ECG/echocardiogram if cardiac involvement suspected.
→ Identify and stop all potential culprit drugs immediately.
→ In Korea, hospitals often perform HLA testing in high-risk populations (e.g., HLA-B*58:01 for allopurinol sensitivity in Koreans).
How it’s Done
→ Step 1: Immediate dechallenge – discontinue all non-essential medications, especially the suspected culprit.
→ Step 2: Initiate systemic therapy – oral or IV corticosteroids as first-line in most moderate-to-severe cases.
→ Step 3: Monitor organ function closely – frequent labs to track liver, kidney, lung, and heart status.
→ Step 4: Supportive skin care – emollients, antihistamines, wound care for erosions.
→ Step 5: Long taper of steroids – usually over 6–12 weeks, since rapid tapering may trigger relapse.
→ Step 6: Consider immunosuppressants (cyclosporine, IVIG) if corticosteroids fail or are contraindicated.
→ Step 7: Long-term follow-up – monitor for late autoimmune complications such as thyroiditis, type 1 diabetes, lupus-like syndromes.
Recovery
→ Acute skin rash and fever typically improve within 1–2 weeks of treatment.
→ Organ involvement may take weeks to months to resolve.
→ Full recovery is possible, but patients may require long-term monitoring for autoimmune diseases.
→ Patients must avoid the culprit drug permanently, with allergy documentation provided for future care.
Complications
→ Acute: hepatitis, nephritis, pneumonitis, myocarditis, encephalitis – which may be fatal.
→ Relapse: often occurs if corticosteroids are tapered too quickly.
→ Late autoimmune disease: thyroid dysfunction, diabetes, lupus-like illness may develop months after recovery.
→ Drug cross-reactivity: patients may react to related drugs (e.g., other aromatic anticonvulsants).
Treatment Options in Korea
→ Korean tertiary hospitals have established DRESS protocols, emphasizing early recognition, immediate dechallenge, and systemic therapy.
→ Systemic corticosteroids are the standard of care, but cyclosporine is increasingly used in severe or steroid-refractory cases.
→ HLA-B*58:01 screening is routinely performed before prescribing allopurinol in Korea, significantly reducing risk.
→ Hospitals provide multidisciplinary care with dermatology, hepatology, nephrology, pulmonology, and cardiology teams as needed.
→ Electronic medical alert systems are used in Korean hospitals to prevent re-prescription of culprit drugs.
→ With this integrated approach, Korea achieves early diagnosis, lower mortality, and structured long-term follow-up for patients recovering from DRESS.