What it is
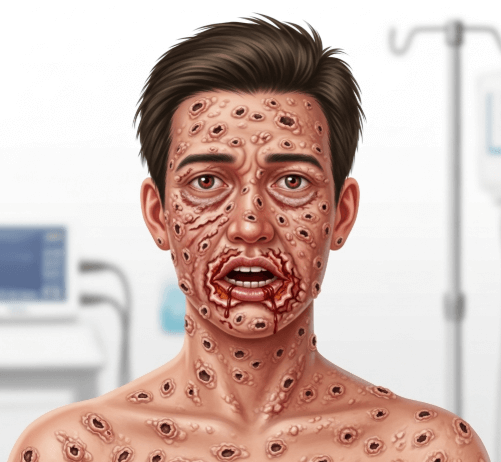
➝ Stevens–Johnson syndrome (SJS) is a rare, severe mucocutaneous reaction, usually to medications, characterized by extensive skin and mucous membrane necrosis and detachment.
➝ It lies on the same spectrum as toxic epidermal necrolysis (TEN), differing mainly by extent of body surface involvement:
- SJS: <10% body surface area (BSA).
- SJS/TEN overlap: 10–30% BSA.
- TEN: >30% BSA.
➝ Common triggers include allopurinol, anticonvulsants, sulfonamides, antibiotics, and NSAIDs.
➝ Triage is essential to ensure rapid withdrawal of the offending drug, supportive stabilization, and early referral to specialized care.
Why it’s done
→ To identify and admit patients quickly, as mortality can reach 10–30% depending on severity.
→ To guide level of care (dermatology vs. ICU/burn unit).
→ To prevent complications such as sepsis, multiorgan failure, or long-term sequelae (ocular, skin, mucosal).
→ In Korea, triage of SJS is streamlined in tertiary hospitals, with rapid referral to burn centers and dermatology teams.
Alternatives to Formal Triage
→ Clinical recognition without scoring: Immediate hospitalization based on skin detachment and mucosal involvement.
→ SCORTEN score: Standardized severity tool used worldwide and in Korea to predict mortality and triage care needs.
→ Multidisciplinary consultation: Dermatology, ophthalmology, ICU, infectious disease, and internal medicine teams.
Preparation
→ Early suspicion is key: patient presents with fever, malaise, sore throat, conjunctivitis, followed by rapidly spreading rash with blistering and mucosal erosions.
→ Medication review: Identify and immediately stop all potential culprit drugs.
→ Baseline investigations: CBC, electrolytes, liver/kidney function, blood cultures, chest X-ray.
→ In Korea, electronic health systems often flag recent high-risk drugs (e.g., allopurinol without HLA-B*58:01 testing).
How it’s Done – Triage Approach
→ Step 1: Immediate drug withdrawal – suspected causative drug must be stopped immediately.
→ Step 2: Assess severity using SCORTEN (within first 24 hours):
- Age >40 years.
- Presence of malignancy.
- Heart rate >120 bpm.
- Initial epidermal detachment >10% BSA.
- Serum urea >10 mmol/L.
- Serum bicarbonate <20 mmol/L.
- Serum glucose >14 mmol/L.
- Each criterion adds risk; higher score = higher mortality.
→ Step 3: Assign level of care
- Mild SJS (<10% BSA, stable): Admit to dermatology ward with close monitoring.
- SJS/TEN overlap or TEN (>10% BSA, unstable vitals, systemic involvement): Admit to ICU or burn unit.
→ Step 4: Specialist involvement
- Dermatology: Primary management.
- Ophthalmology: Early to prevent corneal damage and blindness.
- ENT/urology/gynecology: For mucosal complications.
- Infectious disease: For sepsis prevention.
→ Step 5: Supportive stabilization
- Fluid and electrolyte balance.
- Pain control.
- Nutritional support.
- Strict infection prevention.
Recovery
→ Mortality depends on severity and comorbidities, but early triage improves survival.
→ Skin healing occurs over 2–4 weeks if stabilized, but patients may need long-term ocular and mucosal care.
→ Early ophthalmology intervention in Korea reduces risk of symblepharon and vision loss.
→ Long-term follow-up is required for pigmentation changes, nail loss, scarring, or chronic ocular complications.
Complications
→ Acute: Sepsis, multiorgan failure, fluid/electrolyte imbalance, respiratory distress.
→ Chronic: Ocular damage (dry eye, corneal scarring, blindness), oral/genital mucosal stenosis, nail loss, psychosocial stress.
→ Medication risks: Corticosteroids, cyclosporine, or IVIG may be used in selected cases; risks include infection and delayed wound healing.
Treatment Options in Korea
→ Korean hospitals follow international triage protocols with SCORTEN scoring to determine admission to ICU or burn units.
→ Multidisciplinary care is standard: dermatology, ophthalmology, infectious disease, pulmonology, ICU.
→ Supportive care is prioritized, with systemic therapies (steroids, cyclosporine, IVIG) individualized by case and center.
→ HLA-B*58:01 screening before allopurinol is mandatory in Korea, significantly reducing risk.
→ Major hospitals (Seoul, Busan, Daegu) have dedicated burn/ICU units where severe SJS/TEN patients are transferred.
→ With Korea’s structured triage and referral network, rapid stabilization and specialist input greatly improve survival and reduce complications.