What it is
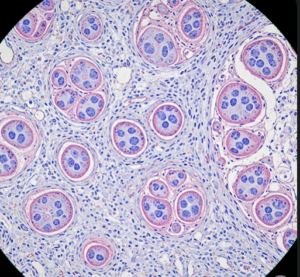
➝ Trichoscopy is a non-invasive, high-resolution imaging technique that uses a dermatoscope or digital video dermatoscope to evaluate the scalp and hair.
➝ It magnifies the scalp surface (10–200×) and allows visualization of hair shafts, follicles, perifollicular structures, and scalp skin changes.
➝ It is now an essential diagnostic and monitoring tool in hair clinics for androgenetic alopecia, alopecia areata, telogen effluvium, cicatricial alopecias, scalp psoriasis, and seborrheic dermatitis.
➝ In Korea, trichoscopy is integrated into dermatology and specialized hair loss clinics, often alongside digital photography, AI-based hair density software, and patient education platforms.
Why it’s done
→ To make an accurate, early diagnosis of different types of hair loss.
→ To monitor disease progression and treatment response over time.
→ To differentiate scarring from non-scarring alopecia, which is crucial for prognosis.
→ To guide treatment decisions (topical vs systemic vs surgical).
→ To provide objective evidence for patients, improving compliance with long-term therapy.
Alternatives
→ Clinical visual inspection: limited sensitivity in early or subtle cases.
→ Scalp biopsy: invasive but sometimes necessary for scarring alopecia.
→ Hair pull and wash tests: crude assessments with limited accuracy.
→ Phototrichogram: useful but requires shaving/scalp marking.
Trichoscopy is considered superior because it is non-invasive, repeatable, and provides immediate results.
Preparation
→ No specific preparation is needed, but patients are advised to wash their hair 24–48 hours before.
→ Avoid topical concealers, fibers, or dyes that may obscure visualization.
→ In Korea, clinics often use standardized lighting, scalp photography booths, and AI-assisted image storage to ensure consistent follow-up comparisons.
How it’s Done
→ A dermatoscope or digital trichoscope is applied to the scalp, often with polarized light or immersion fluid.
→ Key findings vary by condition:
- Androgenetic alopecia: hair diameter variability >20%, miniaturized hairs, yellow dots, peripilar signs.
- Alopecia areata: exclamation mark hairs, black dots, yellow dots, short regrowing hairs.
- Telogen effluvium: uniform hair thinning without miniaturization.
- Scarring alopecia: absence of follicular openings, perifollicular scaling, white patches.
- Seborrheic dermatitis/psoriasis: diffuse scaling, perifollicular redness.
→ Images are stored for baseline comparison and longitudinal follow-up.
→ In Korean clinics, patients are often shown side-by-side before-and-after images to demonstrate progress and reinforce treatment adherence.
Recovery
→ The procedure is painless, non-invasive, and requires no downtime.
→ Patients leave with immediate results and a better understanding of their condition.
→ Long-term, trichoscopy allows tracking of regrowth from therapies like minoxidil, finasteride, JAK inhibitors, PRP, and hair transplantation.
Complications
→ None significant; very safe.
→ Occasionally, false interpretation if hair dyes or scalp products are not cleaned properly.
→ Requires trained dermatologists for accurate reading.
Treatment Options in Korea
→ Trichoscopy is standard in dermatology hospitals, university centers, and private hair loss clinics.
→ Korean clinics often use digital trichoscopy linked with AI-based software to quantify:
- Hair density (hairs/cm²).
- Hair shaft diameter (miniaturization index).
- Vellus-to-terminal hair ratio.
- Scalp health (erythema, scaling, follicular openings).
→ Many clinics integrate trichoscopy into annual or semi-annual hair check-up programs, especially for men and women at risk of androgenetic alopecia.
→ It is also used to plan and track hair transplantation, ensuring donor site evaluation and recipient site density mapping.
→ With Korea’s emphasis on precision dermatology and aesthetic outcomes, trichoscopy is considered a cornerstone diagnostic and monitoring tool in hair medicine.