Overview
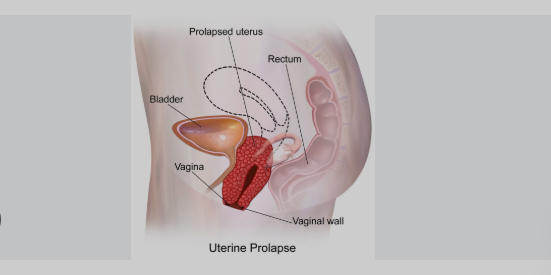
Uterine Prolapse is a condition in which the uterus descends from its normal position into the vaginal canal, often due to weakened pelvic floor muscles and ligaments. It commonly affects women after childbirth or menopause and can range from mild (partial prolapse) to severe (complete prolapse). While not usually life-threatening, it can significantly impact a woman’s quality of life and daily functioning.
What is Uterine Prolapse
Uterine Prolapse occurs when the uterus sags or drops into the vagina due to loss of support from the pelvic floor muscles and connective tissues. The uterus may bulge partially into the vaginal canal (incomplete prolapse) or extend completely outside of it (complete prolapse). It is often associated with aging, vaginal childbirth, and conditions that increase intra-abdominal pressure.
Symptoms
Symptoms vary based on the severity of the prolapse:
- A feeling of heaviness or pressure in the pelvis
- Bulging or protrusion from the vaginal opening
- Urinary incontinence or difficulty emptying the bladder
- Constipation or difficulty with bowel movements
- Vaginal discomfort or pain during intercourse
- Lower back pain
- Recurring urinary tract infections (UTIs)
- Spotting or vaginal bleeding in severe cases
Causes
Uterine prolapse results from the weakening or damage of pelvic floor muscles and ligaments that normally support the uterus. Contributing factors include:
- Vaginal childbirth, especially multiple or difficult deliveries
- Menopause, due to decreased estrogen levels
- Chronic constipation and straining during bowel movements
- Heavy lifting or chronic coughing
- Obesity
- Pelvic tumors or prior pelvic surgery
- Genetic predisposition to connective tissue weakness
Risk Factors
- Age over 50
- Postmenopausal status
- Multiple vaginal births
- Obesity
- Chronic respiratory conditions (e.g., COPD)
- Hysterectomy or prior pelvic surgery
- Family history of pelvic organ prolapse
- Frequent heavy lifting or high-impact exercise
Complications
If left untreated, uterine prolapse may lead to:
- Worsening urinary incontinence or urinary retention
- Recurring bladder infections
- Constipation and bowel dysfunction
- Ulcers or sores on the protruding tissue
- Sexual dysfunction
- Prolapse of other pelvic organs (e.g., bladder or rectum)
- Need for surgical repair or hysterectomy in advanced cases
Prevention
Preventive measures can help reduce the risk or slow the progression of uterine prolapse:
- Perform regular pelvic floor exercises (Kegels)
- Maintain a healthy weight
- Avoid heavy lifting or straining
- Treat and manage chronic cough or constipation
- Use proper lifting techniques
- Hormone therapy (in postmenopausal women, if appropriate)
- Routine pelvic exams for early detection
Treatment Options in Korea
South Korea offers comprehensive and personalized treatment options for uterine prolapse, ranging from conservative approaches to advanced surgical techniques.
- Diagnosis:
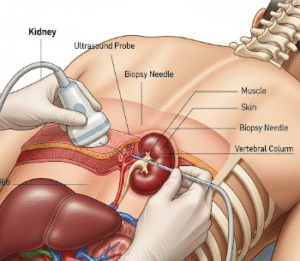
- Pelvic examination
- Ultrasound or MRI for anatomical assessment
- Bladder or bowel function tests, if needed
- Conservative treatments:
- Pelvic floor physical therapy
- Pessary device – a removable vaginal support inserted to hold the uterus in place
- Lifestyle modifications, including weight loss and constipation management
- Estrogen therapy (for postmenopausal women, to improve tissue strength)
- Surgical treatments (for moderate to severe prolapse):
- Vaginal hysterectomy with pelvic floor repair
- Uterine-sparing prolapse surgery (e.g., uterosacral or sacrohysteropexy)
- Laparoscopic or robotic pelvic reconstructive surgery
- Colpocleisis – a vaginal closure procedure for women no longer sexually active
South Korean hospitals provide minimally invasive and fertility-sparing surgical options, advanced recovery protocols, and experienced gynecologic surgeons, ensuring optimal care for women with uterine prolapse.