Overview
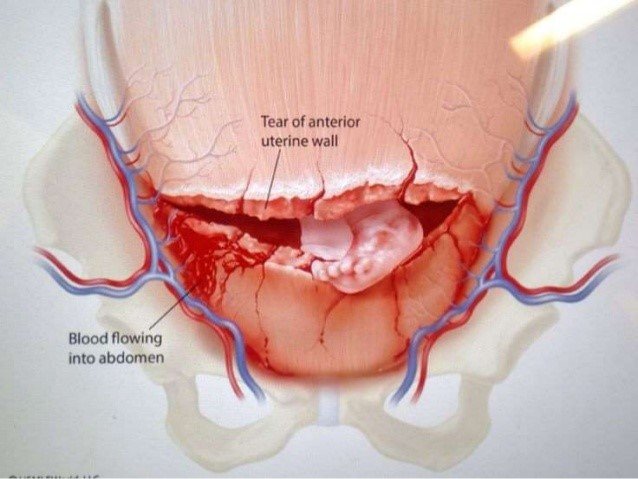
Uterine Rupture is a rare but serious obstetric emergency in which the wall of the uterus tears during pregnancy or labor. It most often occurs in women with a previous cesarean delivery or uterine surgery. This condition poses a significant risk to both the mother and fetus and requires immediate surgical intervention to prevent life-threatening complications.
What is Uterine Rupture
Uterine Rupture is a full-thickness tear in the wall of the uterus, most commonly occurring during labor in women who have a uterine scar from a previous cesarean section or surgery. The rupture allows the fetus, placenta, or amniotic fluid to move into the abdominal cavity, which can lead to massive hemorrhage and fetal distress or death. It is considered a true obstetric emergency and requires rapid diagnosis and surgical response.
Symptoms
Symptoms of uterine rupture can appear suddenly and include:
- Sudden, severe abdominal pain not relieved by contraction rest periods
- Vaginal bleeding
- Loss of uterine tone or a change in the shape of the uterus
- Abnormal fetal heart rate or fetal distress
- Cessation of uterine contractions
- Maternal hypotension (shock)
- Loss of fetal station (baby moves back up in the birth canal)
- Palpable fetal parts in the abdomen (in severe cases)
Causes
The most common causes of uterine rupture include:
- Previous uterine surgery (especially classical cesarean section or myomectomy)
- Trauma to the abdomen during pregnancy
- Prolonged or obstructed labor
- Overuse of labor-inducing medications like oxytocin or prostaglandins
- High parity (multiple prior pregnancies)
- Weakness of the uterine wall from congenital anomalies or infection
Risk Factors
- Previous cesarean delivery (especially with a vertical uterine incision)
- Vaginal birth after cesarean (VBAC)
- History of uterine surgery (e.g., fibroid removal)
- Multiple pregnancies (twins or more)
- Uterine overdistension (e.g., large baby or polyhydramnios)
- Prolonged labor or obstructed labor
- Induction or augmentation of labor with strong uterotonics
- Trauma (e.g., car accident)
Complications
Uterine rupture can result in life-threatening complications for both mother and baby:
- Massive maternal hemorrhage and hypovolemic shock
- Emergency hysterectomy
- Injury to adjacent organs (bladder or bowel)
- Fetal hypoxia, brain injury, or death
- Maternal infection or sepsis
- Uterine scarring and future infertility
- Long-term psychological trauma
Prevention
Though not always preventable, certain measures can reduce the risk of uterine rupture:
- Avoid trial of labor after cesarean (TOLAC) in women with high-risk uterine scars
- Close monitoring during labor, especially in women with uterine surgery history
- Use caution with labor-inducing drugs in women with uterine scars
- Early delivery planning for high-risk pregnancies
- Choosing elective cesarean when vaginal delivery is deemed unsafe
- Prenatal imaging to evaluate scar thickness or uterine abnormalities
Treatment Options in Korea
South Korea provides high-quality emergency obstetric care for uterine rupture through a combination of advanced diagnostics, expert surgical teams, and neonatal intensive care.
- Emergency care:
- Immediate cesarean section to deliver the baby and stop internal bleeding
- Blood transfusions and fluid resuscitation for maternal stabilization
- Surgical repair of the uterine wall, if feasible
- Hysterectomy if the damage is extensive or bleeding cannot be controlled
- Postoperative care:
- ICU monitoring for the mother
- Neonatal intensive care for the newborn if fetal distress occurred
- Follow-up imaging and uterine assessment
- Emotional and psychological counseling after traumatic birth experience
South Korean hospitals are equipped with 24/7 obstetric surgical teams, advanced fetal monitoring, and multidisciplinary emergency care, which are crucial for the successful management of uterine rupture and maternal-fetal survival.