Overview
Urinary Incontinence is the unintentional loss of urine, a condition that affects people of all ages but is most common in older adults, especially women. It ranges from occasional leaks during coughing or exercise to a complete inability to control urination. While not life-threatening, it can significantly affect quality of life, self-esteem, and social interactions. Fortunately, a variety of effective treatments are available.
What is Urinary Incontinence
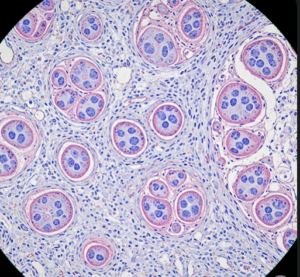
Urinary Incontinence is the loss of bladder control, leading to involuntary leakage of urine. It may be temporary or chronic and can be caused by various underlying conditions. The condition is broadly classified into different types, including stress incontinence, urge incontinence, overflow incontinence, functional incontinence, and mixed incontinence. Accurate diagnosis of the type is crucial to choosing the right treatment.
Symptoms
Symptoms depend on the type of incontinence and its severity:
- Leakage of urine during coughing, sneezing, or exercise (stress incontinence)
- Sudden, uncontrollable urge to urinate followed by leakage (urge incontinence)
- Dribbling of urine due to a full bladder (overflow incontinence)
- Inability to reach the toilet in time (functional incontinence)
- Constant dribbling or dampness in undergarments
- Nighttime urination (nocturia)
- Frequent urination throughout the day
Causes
Urinary incontinence may result from:
- Weak pelvic floor muscles or sphincter dysfunction
- Pregnancy and childbirth
- Menopause and hormonal changes
- Prostate problems (in men)
- Neurological conditions: Parkinson’s, stroke, spinal cord injury
- Urinary tract infections
- Bladder stones or tumors
- Medications: diuretics, sedatives, muscle relaxants
- Chronic constipation or obesity
Risk Factors
- Female sex (especially post-pregnancy or postmenopausal)
- Age (risk increases with age)
- Obesity
- Smoking
- Diabetes
- Family history of incontinence
- Neurological conditions
- Pelvic surgery
Complications
Untreated or poorly managed urinary incontinence can lead to:
- Skin irritation or infections
- Urinary tract infections (UTIs)
- Emotional distress and depression
- Sleep disturbances
- Avoidance of social activities
- Reduced quality of life
- Risk of falls in older adults rushing to the toilet
Prevention
While not always preventable, the risk of urinary incontinence can be reduced by:
- Pelvic floor (Kegel) exercises to strengthen bladder muscles
- Maintaining a healthy weight
- Avoiding bladder irritants (e.g., caffeine, alcohol, spicy foods)
- Treating constipation promptly
- Practicing bladder training
- Controlling blood sugar levels in diabetic patients
- Avoiding smoking, which weakens pelvic muscles and increases coughing
Treatment Options in Korea
South Korea offers advanced and multidisciplinary treatment approaches for urinary incontinence, addressing both the physical and psychological aspects:
- Accurate diagnosis through:
- Urodynamic studies
- Bladder diaries
- Cystoscopy and pelvic exams
- Conservative treatments:
- Pelvic floor muscle training
- Bladder training and timed voiding
- Dietary modifications
- Medications:
- Anticholinergics for urge incontinence
- Beta-3 adrenergic agonists to relax the bladder
- Topical estrogen in postmenopausal women
- Minimally invasive procedures:
- Botulinum toxin (Botox) injections into the bladder wall
- Nerve stimulation therapy (e.g., sacral neuromodulation, tibial nerve stimulation)
- Surgical options:
- Mid-urethral sling procedures for stress incontinence
- Urethral bulking agents