Overview
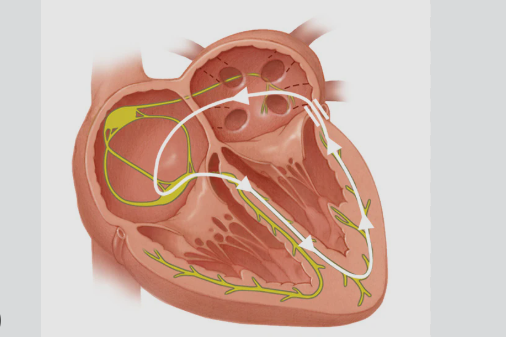
Wolff-Parkinson-White Syndrome (WPW) is a rare congenital heart condition that causes episodes of rapid heart rate (tachycardia) due to an extra electrical pathway in the heart. This abnormal pathway allows electrical signals to bypass the normal route, leading to arrhythmias. While WPW can be asymptomatic, it may lead to palpitations, dizziness, or even sudden cardiac arrest in rare cases. With proper diagnosis and treatment, most people with WPW live healthy lives.
What is Wolff-Parkinson-White Syndrome?
WPW is a type of pre-excitation syndrome caused by the presence of an extra electrical conduction pathway, known as the Bundle of Kent, between the atria and ventricles. This allows electrical impulses to travel abnormally, sometimes triggering episodes of supraventricular tachycardia (SVT). WPW is typically present from birth but may not cause symptoms until adolescence or adulthood. It is diagnosed through a characteristic ECG pattern and managed depending on the severity of symptoms.
Symptoms
Not everyone with WPW experiences symptoms, but when they occur, they often include:
- Sudden rapid heartbeats (palpitations)
- Dizziness or lightheadedness
- Shortness of breath
- Chest discomfort or pressure
- Fainting (syncope)
- Fatigue during physical activity
- In infants: rapid breathing, poor feeding, or irritability
Episodes may last seconds to hours and can occur sporadically or frequently.
Causes
WPW is caused by a congenital abnormality, meaning the person is born with an extra electrical connection between the upper and lower chambers of the heart.
- This accessory pathway bypasses the AV node, disrupting normal electrical conduction.
- In rare cases, WPW can be inherited in an autosomal dominant pattern.
- It may occur alone or with other congenital heart diseases like Ebstein’s anomaly.
Risk Factors
Factors that increase the likelihood of WPW include:
- Family history of WPW or arrhythmias
- Congenital heart defects
- Male gender (slightly more common)
- Infancy or young adulthood, which is when symptoms typically emerge
- Genetic mutations associated with inherited WPW (rare cases)
Complications
Although many people with WPW live symptom-free, complications can occur if the condition is not managed properly:
- Paroxysmal supraventricular tachycardia (PSVT)
- Atrial fibrillation with very fast ventricular rates
- Sudden cardiac arrest, although very rare
- Heart failure in severe or prolonged arrhythmic episodes
- Decreased quality of life due to frequent symptoms
Immediate treatment during an attack is critical to avoid complications.
Prevention
WPW Syndrome cannot be prevented, as it is congenital. However, the risk of complications can be minimized through:
- Early diagnosis via ECG if symptoms arise
- Avoidance of stimulants like caffeine, alcohol, or certain medications that can trigger arrhythmias
- Prompt treatment of associated arrhythmias such as atrial fibrillation
- Regular cardiology check-ups, especially for symptomatic individuals
- Genetic counseling in families with a known hereditary form
Treatment Options in Korea
South Korea offers state-of-the-art cardiology care for arrhythmias such as WPW Syndrome, including diagnostics, medication, and interventional procedures. Key treatment options include:
- Electrocardiogram (ECG) and electrophysiology studies (EPS) for precise diagnosis
- Antiarrhythmic medications like beta-blockers or Class IC/III drugs for symptom control
- Radiofrequency catheter ablation (RFA) – a curative, minimally invasive procedure that destroys the abnormal pathway
- Vagal maneuvers or adenosine injections for acute episode termination
- Implantable cardioverter-defibrillator (ICD) – rarely needed but considered for high-risk patients
- Advanced cardiology departments at Asan Medical Center, Samsung Medical Center, Seoul National University Hospital, and Yonsei Severance Hospital offer expert electrophysiology teams with excellent outcomes in WPW ablation procedures