What it is
Intensive care refers to specialized medical care provided to patients with life-threatening conditions or severe illnesses. It is delivered in a Hospital Intensive Care Unit (ICU), where patients receive constant monitoring, advanced medical support, and multidisciplinary care.
Key points:
- Designed for patients with critical health conditions such as severe infections, trauma, heart attack, respiratory failure, or organ dysfunction.
- Equipped with advanced monitoring devices, ventilators, dialysis machines, and life-support systems.
- Care is provided by a multidisciplinary team including intensivists, nurses, respiratory therapists, and other specialists.
- Emphasis on continuous monitoring, rapid intervention, and stabilization of vital functions.
Why it’s done
Patients are admitted to intensive care for several reasons:
- Respiratory failure: Need for mechanical ventilation or advanced oxygen therapy.
- Cardiovascular instability: Severe heart conditions, shock, or post-heart surgery recovery.
- Sepsis or severe infections: Life-threatening infections requiring constant monitoring and intravenous therapies.
- Major surgery recovery: Complex surgical procedures requiring close observation.
- Multi-organ failure: Monitoring and support for liver, kidney, or heart dysfunction.
- Trauma and accidents: Severe injuries from accidents or falls.
Note: Intensive care is critical for stabilizing patients, preventing complications, and improving survival chances.
Alternatives
Alternatives or complementary care options depend on the patient’s condition:
- High-dependency units (HDU): For patients needing monitoring but not full ICU-level care.
- Step-down units: Intermediate care for patients recovering from ICU.
- Regular hospital wards: Suitable for stable patients who do not require intensive monitoring.
- Home care with oxygen or monitoring: Only for non-critical conditions with minimal support needs.
Important: For critically ill patients, ICU care is often irreplaceable. Alternatives may be used once the patient stabilizes.
Preparation
Preparation for ICU admission depends on the situation:
- Emergent admission: Rapid assessment, stabilization of vital signs, and initiation of monitoring.
- Planned admission (post-surgery): Preoperative evaluation, consent, and briefing on ICU care.
- Family preparation: Understanding visitation rules, care protocols, and communication procedures.
- Patient preparation: Ensure medications, medical history, and identification are available.
Patient instructions (if planned):
- Discuss any allergies or chronic conditions with medical staff.
- Arrange advance directives or consent for life-support interventions if applicable.
- Family should prepare personal items for ICU stay (glasses, hearing aids, etc.).
How it’s done
Intensive care involves continuous monitoring and active treatment:
1. Monitoring:
- Vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) are tracked continuously.
- Advanced monitoring for ECG, central venous pressure, intracranial pressure, and urine output.
2. Life-support interventions:
- Mechanical ventilation for patients unable to breathe independently.
- Dialysis for kidney failure.
- Vasopressors and inotropes for blood pressure support.
- Intravenous medications, nutrition, and fluids to stabilize metabolism.
3. Specialized care:
- Multidisciplinary team manages infection control, sedation, pain, wound care, and nutrition.
- Regular imaging and laboratory tests guide treatment decisions.
- Continuous adjustment of therapies based on patient response.
Duration: ICU stay varies from hours to weeks, depending on illness severity.
Recovery
Recovery in ICU is gradual and closely monitored:
- Stabilization phase: Vital signs normalized, organ support reduced gradually.
- Transition phase: Patients may move to HDU or general wards once stable.
- Rehabilitation phase: Physical therapy, respiratory therapy, and psychological support.
- Follow-up: Ongoing outpatient care may be required for organ function, mobility, and mental health.
Benefits of recovery:
- Survival from life-threatening illness or trauma.
- Prevention of secondary complications such as infections or organ failure.
- Structured rehabilitation improves long-term quality of life.
Complications
ICU care can have potential risks, including:
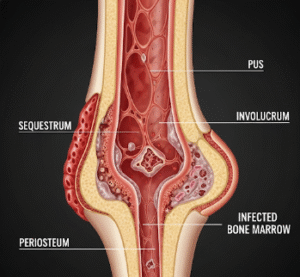
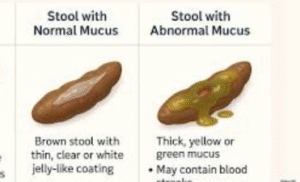
- Infections: Ventilator-associated pneumonia, catheter-related infections.
- Delirium or cognitive issues: Due to sedation, stress, or prolonged ICU stay.
- Muscle weakness or atrophy: From immobility.
- Organ dysfunction: Potential for secondary organ stress during critical illness.
- Emotional impact: Anxiety, depression, or PTSD in patients and families.
Prevention:
- Strict infection control and hygiene protocols.
- Early mobilization and physical therapy.
- Family communication and psychological support for patients.
- Regular evaluation and adjustment of medications and life-support interventions.
Treatment Options in Korea
Intensive care in Korea is highly advanced, with world-class facilities in public and private hospitals:
Key features:
- ICUs are equipped with modern ventilators, dialysis machines, monitoring systems, and life-support equipment.
- Staffed by trained intensivists, nurses, respiratory therapists, and multidisciplinary teams.
- Available for medical, surgical, trauma, and cardiac patients.
- Hospitals follow international ICU standards for safety, monitoring, and infection control.
- Families receive clear guidance, regular updates, and support services during ICU stay.
Summary: Intensive care in Korea provides critical life-saving treatment for severely ill patients. Through advanced monitoring, multidisciplinary care, and specialized interventions, ICUs help stabilize, treat, and rehabilitate patients with serious medical conditions.