What it is
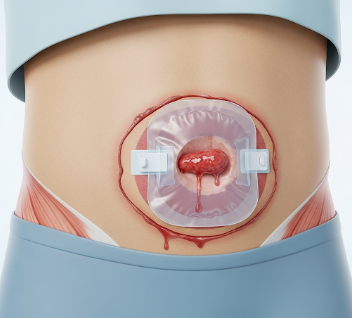
An ileostomy is a surgical procedure that creates an opening (stoma) in the abdominal wall through which the end of the small intestine (ileum) is brought to the surface. This allows waste (stool) to exit the body into a special pouch or bag, bypassing the colon and rectum.
Key points:
- Can be temporary or permanent, depending on the underlying condition.
- Waste is collected in an external ileostomy bag, which needs to be emptied and changed regularly.
- Typically performed when the colon, rectum, or anus cannot safely function.
- Supports patients with conditions like Crohn’s disease, ulcerative colitis, or colorectal cancer.
Why it’s done
Ileostomy is recommended for several medical reasons:
- Inflammatory bowel disease (IBD): Severe Crohn’s disease or ulcerative colitis not controlled by medication.
- Colorectal cancer: When the lower bowel must be bypassed due to tumor removal.
- Trauma or injury: Damage to the bowel requiring temporary diversion.
- Congenital conditions: Rare malformations affecting bowel function.
- Chronic bowel obstruction or infection: When fecal diversion is necessary to allow healing.
Note: The decision for ileostomy depends on disease severity, bowel health, and surgical goals.
Alternatives
Before ileostomy, alternatives may include:
- Medical therapy: Anti-inflammatory drugs, biologics, or immunosuppressants for IBD.
- Colorectal surgery without stoma: For suitable patients, bowel reconnection may be possible.
- Temporary colostomy: Depending on the location of the disease or injury.
- Minimally invasive bowel procedures: Endoscopic interventions or resection for localized issues.
Important: Alternatives are considered based on disease location, patient condition, and potential complications.
Preparation
Proper preparation ensures safety, comfort, and optimal outcomes:
- Preoperative evaluation: Blood tests, imaging (CT, MRI), and anesthesia assessment.
- Stoma site marking: A stoma care nurse determines the best location on the abdomen for easy pouch attachment.
- Dietary preparation: Patients may need low-residue diets or bowel cleansing before surgery.
- Medication review: Adjust anticoagulants or other medications as advised.
- Informed consent: Understanding procedure, stoma care, and lifestyle adjustments.
Patient instructions:
- Arrange for postoperative support at home.
- Learn basic stoma care techniques from nurses or educational resources.
- Prepare clothing and supplies compatible with ileostomy pouching.
How it’s done
Ileostomy is performed under general anesthesia:
- The surgeon identifies the terminal ileum (end of the small intestine).
- A small opening is created on the abdominal wall, usually on the right lower quadrant.
- The ileum is brought through the opening and folded slightly to form a stoma.
- The stoma is secured, and an external ileostomy bag is attached.
- Surgery may be open (traditional) or laparoscopic (minimally invasive).
Types of ileostomy:
- Loop ileostomy: A temporary stoma created to divert stool and allow healing.
- End ileostomy: Permanent stoma after removal of the colon or rectum.
Duration: Surgery usually takes 1–3 hours, depending on complexity.
Recovery
Recovery after ileostomy involves wound healing, adaptation, and learning stoma care:
- Hospital stay: Typically 3–7 days, depending on patient health and type of surgery.
- Initial recovery: Mild pain, swelling, or discharge around stoma; managed with medications.
- Dietary adjustments: Begin with liquids, then progress to soft foods as tolerated.
- Stoma care: Learning to empty, clean, and change the pouch is crucial.
- Follow-up: Regular visits with a surgeon and stoma care nurse to monitor healing and adaptation.
Benefits of recovery:
- Relief from bowel obstruction, disease symptoms, or infection risk.
- Improved quality of life after successful adaptation to stoma care.
- Enables ongoing medical treatments without interruption.
Complications
Ileostomy carries potential risks:
- Stoma complications: Retraction, prolapse, irritation, or infection.
- Skin issues: Contact dermatitis or breakdown from pouch leakage.
- Bowel obstruction: Rare, can occur post-surgery.
- Dehydration: High-output stomas may lead to fluid and electrolyte imbalance.
- Psychological impact: Anxiety, depression, or adjustment difficulties.
Prevention:
- Proper stoma site selection and surgical technique.
- Learn correct stoma care and pouching methods.
- Maintain hydration and nutrition.
- Regular follow-ups with surgeons and stoma care specialists.
Treatment Options in Korea
Ileostomy is a well-established procedure in Korean hospitals and specialized gastrointestinal centers:
Key features:
- Performed in general hospitals, colorectal surgery units, and IBD specialty clinics.
- Both temporary and permanent ileostomies are available.
- Korean hospitals provide stoma care education, follow-up programs, and support groups.
- Minimally invasive laparoscopic ileostomy is widely practiced for faster recovery and less scarring.
- Postoperative care includes dietary counseling, psychological support, and complication monitoring.
Summary: Ileostomy in Korea is a safe, effective procedure for diverting stool in patients with colorectal disease or bowel dysfunction. With proper surgical technique, stoma care, and support, patients can adapt to lifestyle changes, manage symptoms, and maintain quality of life.